What is achilles tendonopathy?
The muscle group at the back of your lower leg is commonly
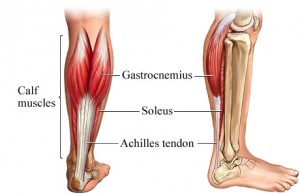 called the calf. The calf comprises 2 major muscles, one of which originates from above the knee joint – the gastrocnemius. The other originates from below the knee joint – the soleus. Both of these muscles insert into the heel bone via the Achilles tendon.
called the calf. The calf comprises 2 major muscles, one of which originates from above the knee joint – the gastrocnemius. The other originates from below the knee joint – the soleus. Both of these muscles insert into the heel bone via the Achilles tendon.
During contraction of the calf, tension is placed through the achilles tendon. When this tension is excessive due to too much repetition or high force, damage to the tendon occurs. Achilles tendinopathy is a condition whereby there is damage to the tendon with subsequent degeneration.
This may occur traumatically due to a high force going through the tendon beyond what it can withstand or due to gradual wear and tear associated with overuse. Patients with achilles tendinopathies typically experience pain during activities requiring strong calf contractions such as running (especially uphill), jumping and hopping.
.
What factors predispose you to getting an achilles tendonopathy?
There are several factors which can predispose patients to developing this condition. These need to be assessed and corrected with direction from your physiotherapist. Some of the factors which contribute to the development of this condition include: poor flexibility, inappropriate training, poor foot biomechanics, inadequate warm up and muscle weakness.
.
What is the treatment for an achilles tendinopathy?
Most patients with achilles tendinopathies heal well with an appropriate physiotherapy program. This can be a lengthy process and may take up to 6 months in patients who have their condition for a long period of time. Early physiotherapy treatment is vital to hasten recovery.
The success rate of the physiotherapy program is largely dictated by patient compliance with the program. One of the key components of the program in the early stages is that you unload the tendon sufficiently (tape, heel wedges, orthotics). This allows your body to begin the healing process in the absence of further tissue damage. Once this is achieved you should have a gradual return to these activities in a progressive manner increasing the load gradually.
Regular icing and anti-inflammatory medication may help to significantly reduce inflammation in the initial phase of this condition. A graduated flexibility and eccentric strength program under direction from your physiotherapist is vital to ensure an optimal outcome.
Physiotherapy can hasten the healing process and may involve: soft tissue massage, electrotherapy (e.g. ultrasound, although there is no conclusive research to support this modality), anti-inflammatory medication, the use of heel wedges, joint mobilization, ice / heat treatment, home exercises to improve strength and flexibility, education, activity modification advice, biomechanics correction.
Despite appropriate physiotherapy management, some patients with this condition do not improve. When this occurs your physiotherapist or doctor will advise you on the best course of management. This may include pharmaceutical intervention, corticosteroid injection or referral to appropriate medical authorities who will advise on any interventions that may be appropriate to improve your condition.
.

